Addressing Nerve Damage Caused by Type 2 Diabetes
Diabetes, particularly Type 2, is a widespread condition affecting millions worldwide. One of its severe complications is nerve damage, known as diabetic neuropathy, which can significantly impact a person’s quality of life. This blog will explore the causes, symptoms, and strategies to address and manage nerve damage caused by Type 2 diabetes.
Understanding Diabetic Neuropathy
Diabetic neuropathy occurs when high blood sugar levels damage nerves throughout the body. It primarily affects the legs and feet but can also impact other areas. There are several types of diabetic neuropathy, including:
- Peripheral Neuropathy: The most common type, affecting the feet and legs, and sometimes the hands and arms.
- Autonomic Neuropathy: Affects the nerves controlling internal organs, leading to issues with the digestive system, bladder, and heart.
- Proximal Neuropathy: Causes pain in the hips, thighs, or buttocks and can lead to leg weakness.
- Focal Neuropathy: Sudden weakness of one nerve or a group of nerves, causing muscle weakness or pain.
Causes of Diabetic Neuropathy
Chronic high blood sugar levels are the primary cause of diabetic neuropathy. Other contributing factors include:
- Inflammation: Inflammation in the nerves can lead to nerve damage.
- Genetics: Some individuals may be genetically predisposed to nerve damage.
- Lifestyle Factors: Unhealthy diet, lack of exercise, and smoking can exacerbate nerve damage.
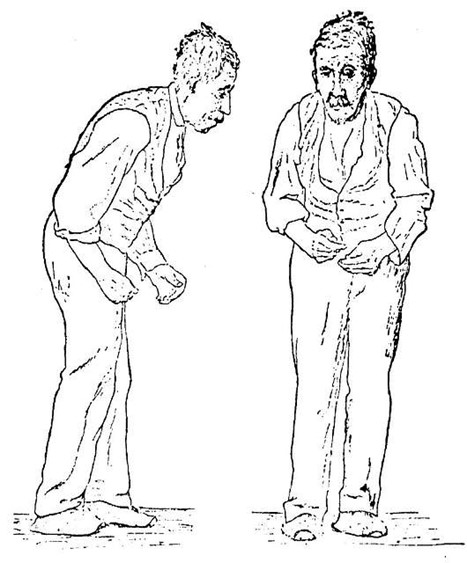
Symptoms of Diabetic Neuropathy
Symptoms vary depending on the type of neuropathy but can include:
- Peripheral Neuropathy: Numbness, tingling, or burning sensation in the feet and hands, extreme sensitivity to touch, and muscle weakness.
- Autonomic Neuropathy: Digestive issues, urinary problems, sexual dysfunction, and abnormal heart rate or blood pressure.
- Proximal Neuropathy: Severe pain in the hip, thigh, or buttock, leading to muscle weakness.
- Focal Neuropathy: Sudden weakness or pain in a specific nerve, such as in the hand, head, or torso.
Strategies to Address and Manage Nerve Damage
- Blood Sugar Control
Maintaining optimal blood sugar levels is crucial in preventing further nerve damage. Regular monitoring and following a diabetes management plan can help achieve this.
- Medications
Various medications can help manage pain and symptoms of diabetic neuropathy, including pain relievers, antidepressants, and anti-seizure drugs.
- Lifestyle Modifications
A healthy diet, regular exercise, and quitting smoking are essential in managing diabetes and reducing the risk of nerve damage.
- Physical Therapy
Physical therapy can help manage pain, improve mobility, and strengthen muscles.
- Alternative Therapies
Some individuals find relief through acupuncture, biofeedback, or supplements like alpha-lipoic acid and vitamin B12.
- Regular Check-Ups
Regular visits to a healthcare provider for check-ups and monitoring can help manage the condition effectively.
To learn more, check out this summary from University Hospitals.
By understanding the condition and taking proactive steps, individuals with diabetes can manage neuropathy and improve their quality of life. If you or a loved one is dealing with diabetic neuropathy, consult with healthcare professionals to create a personalized management plan.
Elevate your well-being with GlucoSupreme Herbal, an advanced supplement crafted by the esteemed Asher Longevity Institute. This exceptional formula not only promotes optimal blood glucose levels but also proves indispensable for those striving to attain their ideal weight and efficiently manage lipid levels.